Summary
This page provides a calculator for estimating the expected productivity cost resulting from the risk of getting Lyme disease based on where you live in the USA. (Other countries aren't supported.) The calculator itself appears first, and the rest of this page explains the parameters and adds other commentary.
The numbers in this calculator aren't solid (that's why you can change the inputs), and I welcome corrections.
Contents
Calculator parameters and results
Risk
| Variable symbol | Parameter name | Value |
| State | ||
| County | ||
| C | Cases (confirmed + probable) per year (average of years 2008 to 2014) | |
| P | County population in 2013 | |
| N = C/P | Naive annual infection probability (cases per 100,000 per year) | |
| R | (actual cases) / (reported cases) | |
| M | Risk multiplier for your particular case | |
| A = N * R * M | Actual annual infection probability (cases per 100,000) |
Expected productivity loss from Lyme disease
| Variable symbol | Parameter name | Value |
| p1m | Prob(symptoms last >= 1 month) | |
| p3m | Prob(symptoms last >= 3 months) | |
| p6m | Prob(symptoms last >= 6 months) | |
| p1y | Prob(symptoms last >= 1 year) | |
| p5y | Prob(symptoms last >= 5 years) | |
| p10y | Prob(symptoms last >= 10 years) | |
| p20y | Prob(symptoms last ~20 years) | |
| S1m | (your productivity with symptoms) / (your regular productivity) during first month of Lyme | |
| S1y | (your productivity with symptoms) / (your regular productivity) during first year of Lyme after the first month | |
| S>1y | (your productivity with symptoms) / (your regular productivity) during PTLDS after first year of Lyme | |
| La | Expected productive years of life lost per infection | |
| A * L | Expected days of life lost per year (i.e., risk of infection per year times expected cost of infection) |
Time spent checking for ticks
| Variable symbol | Parameter name | Value |
| T | Minutes lost to check for ticks once | |
| Y | Number of times you check for ticks per year (probably <365 because there aren't many ticks in winter—see "Cases by Month" here) | |
| H | Number of hours per day during which you get things done (not sleeping, showering, etc.) | |
| D = Y * (T/60)/H | Days spent checking ticks per year |
Total time cost per year
Expected days lost per year due to morbidity and checking ticks = .
Explanation of the parameters
Risk
C
 The data on cases of Lyme disease by state and county are taken from CDC's website, namely, this data set, which I copied onto my own site in case the original disappears. It provides counts of Lyme-disease cases by county from 2000 to 2014. By comparing the 2014 case counts to statewide totals, I deduce that these are counts of confirmed + probable cases (at least starting in 2008 when CDC began counting probable cases). I deduce this because the statewide totals page gives 25,359 confirmed and 8102 probable cases, which adds to 33,461, which exactly matches the 2014 total (summed over all counties in all states) in the county-level dataset.
The data on cases of Lyme disease by state and county are taken from CDC's website, namely, this data set, which I copied onto my own site in case the original disappears. It provides counts of Lyme-disease cases by county from 2000 to 2014. By comparing the 2014 case counts to statewide totals, I deduce that these are counts of confirmed + probable cases (at least starting in 2008 when CDC began counting probable cases). I deduce this because the statewide totals page gives 25,359 confirmed and 8102 probable cases, which adds to 33,461, which exactly matches the 2014 total (summed over all counties in all states) in the county-level dataset.
Rather than just counting 2014 cases (the most recent year available), I took an average of cases between 2008 and 2014, in order to get a bigger sample over time, since some counties have no cases in 2014 but a few cases in previous years. I could have gone all the way back to 2000, but since incidence of Lyme disease has been growing/changing rapidly in recent decades, I didn't want to go back too far.
If you live in a small county, the sample size might still be rather small, so you could also look at statistics for neighboring counties. Likewise, because I didn't spend a lot of time cleaning the data, there may be a few counties missing data. If that's true for you, you too can look at neighboring areas to get a guess about your risk, or look at CDC's map.
P
Incidence proportion is (new cases per year)/population. So to calculate Lyme-disease risk, I needed the populations of US counties. I tried to get this information from the US Census website, but downloading the data was taking forever and seemed stuck. So instead I used data from Wikipedia. I copy-pasted Wikipedia's table into a text file and uploaded it to my site.
There are a few counties for which my calculator doesn't work, usually due to edge cases of formatting in the input files. In such instances, you can look up the numbers manually.
N
Based only on the C and P parameters, we would naively calculate the incidence proportion as C/P. As the CDC does, I show this number in cases per 100,000 people in the population per year, which is a layperson-friendly way of saying that the number should be multiplied by 10-5 to get the actual probability.
If you compute values of N for various counties within a state using this calculator, the average of the results tends to be somewhere in the ballpark of the statewide average incidence rate as reported here, which gives some confidence that my calculations aren't way off due to an error. Of course, if you find particular numbers that seem weird, let me know.
R
CDC reports 25,359 confirmed and 8102 probable cases of Lyme disease in 2014, or a total of 33,461. CDC's page of caveats about the data mentions that "Not every case of Lyme disease is reported to CDC". In fact, it looks like this is quite an understatement. Another page on CDC's site explains that, using alternate methods of assessing Lyme incidence, "the number of people diagnosed with Lyme disease each year in the United States is around 300,000"—almost 10 times higher than the cases reported to CDC.
The 300,000 number is based on an estimate of "people who tested positive for Lyme disease" and an alternative estimate of "people diagnosed with Lyme disease". But of course, both of these measures may also underestimate the true number of infections, since some people may never see a doctor.
Tests may have false negatives (though they may also have false positives). Regarding Lyme testing: "The overall rate of false positives is low, only about 1 to 3%, in comparison to a false-negative rate of up to 36% in the early stages of infection using two-tiered testing.[97]" Assuming that, of those people who get tested, the fraction who actually have Lyme disease isn't very close to 0%b, this suggests that more people wrongly test negative than wrongly test positive. Presumably this should somewhat increase our estimate of the actual number of infections, though I haven't delved into the fine print of this research enough to know the answer.
To correct for these problems, I multiply the naive incidence proportion by a factor of R to get the true incidence proportion. This is a hacky correction, but it probably preserves some truth when comparing different regions of the US, because CDC says that underreporting of Lyme cases
do[es] not affect our understanding of the geographic distribution of Lyme disease. Lyme disease cases are concentrated in the Northeast and upper Midwest, with 14 states accounting for over 96% of cases reported to CDC. The results obtained using the new estimation methods mirror the geographic distribution of cases that is shown by national surveillance.
My calculator doesn't consider other tick-borne diseases besides Lyme, since "Other pathogens are much more rare" than the bacterium that causes Lyme disease. As a kludgey way to account for other tick-borne diseases, I slightly increased R, but I don't know how much of an increase is appropriate. This section reports: "Among early Lyme disease patients, depending on their location, 2–12% will also have HGA and 2–40% will have babesiosis.[65]" Are the symptoms of these coinfections included in the symptomatology that people report for Lyme-disease cases, in which case the harm caused by these coinfections is "already counted" by reports of what some Lyme patients experience? Or are the effects of these coinfections reported separately, in which case I should add on their expected harm to the expected harm of Lyme itself in my calculations? Of course, in cases where non-Lyme tick-borne infections occur without Lyme, the afflictions caused by non-Lyme diseases aren't "already counted" in reports of Lyme symptoms.
One person who lives in Albany County, New York told me in 2017 that she knows of ~5 people who have gotten Lyme disease in the last ~5 years, and she probably would know whether someone had gotten Lyme disease for ~100 of her friends. That suggests roughly a 1%/year risk of Lyme in this area. And indeed, my calculator reports that N * R for Albany County, New York is about 1000 cases per 100,000, or about 1% per year.
Olivier (2017) reports:
Holly Ahern, an associate professor of microbiology at the State University of New York (SUNY) Adirondack[...] figures new cases of Lyme disease are more likely [...] closer to 700,000 per year. She says that's because the blood tests for Lyme, upon which the CDC’s statistics are based, have a sensitivity rate of less than 50 percent. "This means that for every two people who have Lyme disease, only one person will be diagnosed as having it. This leaves the other 50 percent without a diagnosis, and therefore without effective treatment," Ahern says. "It is not just the fastest growing vector-borne disease, it is already the second most common infectious disease, right after chlamydia, and ahead of gonorrhea."
I've stuck with a lower R value to be conservative, but if Ahern is right, it should be higher.
M
Your personal risk of Lyme disease may be many times different than your county-wide risk. You can express information about this in the M parameter, since the final risk amount, A, is computed as N * R * M.
Your risk is higher if you
- Go outdoors often, especially in tall grass or woods. (Walking outside crushes tons of bugs, so I discourage walking outside anyway.)
- Live in a rural area, surrounded by lots of vegetation. (In particular, M is bigger if you live in a more rural area than average in your county. If you live in a rural area but a less rural area than most other people in your county, your M might need to be less than 1.)
- Have a pet who might bring ticks inside.
- Don't check for ticks very often.
I live almost entirely indoors, which helps lower my risk, but as of 2016, I live in a very secluded, woody area, which is teeming with ticks. In fact, one morning in July 2016, I walked onto the wooden step outside my front door, and within ~15 seconds, I had a tick crawling up my leg. My housemate spends a lot more time outside and finds 0-2 ticks on their body each year. Two close relatives of mine who live nearby (one of them being my dad) have both been given antibiotics in response to tick bites in the last few years. So Lyme disease is far from a theoretical risk for me, which is why I wanted to research it more in the first place.
I've found about one tick crawling on me each year since I've been in Albany County, New York, but fortunately "Only 1% to 2% of people who are bitten by a tick are at risk for getting the disease." Wikipedia echoes that "transmission is quite rare, with only about 1% of recognized tick bites resulting in Lyme disease." This page reports that "In most places in the US, 30-50% of deer ticks will be infected with Borrelia burgdorferi (the agent of Lyme disease)." Seeker (2015): "According to Paul Mead, Chief of Epidemiology & Surveillance Activity at the CDC, one out of every four or five ticks might be infected in areas where the disease is very common" (0m39s into the video).
Expected productivity loss from Lyme disease
This section includes parameters to roughly specify a probability distribution for how long Lyme symptoms last. I unfortunately don't have great data on this, so I'm making up several of the estimates, but I'm trying to fit them within a few data points that I do have information about.
p1m
Lyme-disease "Treatment is usually for two or three weeks.[1]" I rounded this up to one month and assumed that symptoms last during this time period, though obviously this varies from person to person.
p6m
Wikipedia explains: "Despite appropriate treatment, about 10 to 20% of people develop joint pains, memory problems, and feel tired for at least six months.[2][3]" This is what's called Post-Treatment Lyme Disease Syndrome (PTLDS). This is a condition recognized by mainstream medicine, in contrast to "Chronic Lyme disease".
This article reports:
Early investigators observed that patients with early or late-stage Lyme disease may have lingering symptoms after completion of antibiotic therapy, despite prompt administration of effective antibiotic therapy and resolution of the physical findings of infection.5–7 The frequency of PTLDS among such patients has been found to differ between 0% and 50% in published studies, and is likely related to variability of study design and enrollment criteria of the sample populations used.5,8 Reports of long-term follow-up in patients with early presentation and treatment of EM have generally shown excellent long-term outcomes.1 In the most recent treatment trials of EM conducted in North America, rates of PTLDS are approximately 10% to 20%.3 However, rates may be 50% in the community practice of medicine, where delayed diagnosis and treatment may be more common and classification of symptoms attributed to Lyme disease less certain.9,10
This study found that out of 74 patients with confirmed Lyme disease, 43 (60%) returned to their usual health within 6 months of treatment, 20 (28%) "had either residual symptoms or functional impact, but not both, and did not meet criteria for PTLDS", and 8 (11%) "met our operationalized definition of PTLDS, which included self-reported symptoms of fatigue, widespread musculoskeletal pain or cognitive complaints, and functional impact".
This study found that after Lyme treatment:
At 6 months, 36% of patients reported new-onset fatigue, 20% widespread pain, and 45% neurocognitive difficulties. However, less than 10% reported greater than “minimal” depression across the entire period.
This study says
In 8 studies of patients with EM, the frequency of PTLDS at ≥6 months after treatment varied from 0% to 40.8%, with a median value of 11.5% [2]. In an unknown proportion of patients, such symptoms are so severe that they interfere with functionality, which has been referred to by some authorities as post-treatment Lyme disease syndrome [1].
This page says:
Up to one third of Lyme disease patients who have completed a course of antibiotic treatment continue to have symptoms, often termed "post-Lyme syndrome", such as severe fatigue, sleep disturbance, unconsciousness, and cognitive difficulties, with these symptoms being severe in about 2% of cases.[8][9]
p1y, p5y, p10y, and p20y
This study followed 128 patients "with culture-confirmed early Lyme disease" (p. 1) prospectively for many years. "Fourteen (10.9%) were regarded as having possible PTLDS" (p. 1). The following table shows what happened to these 14 patients.
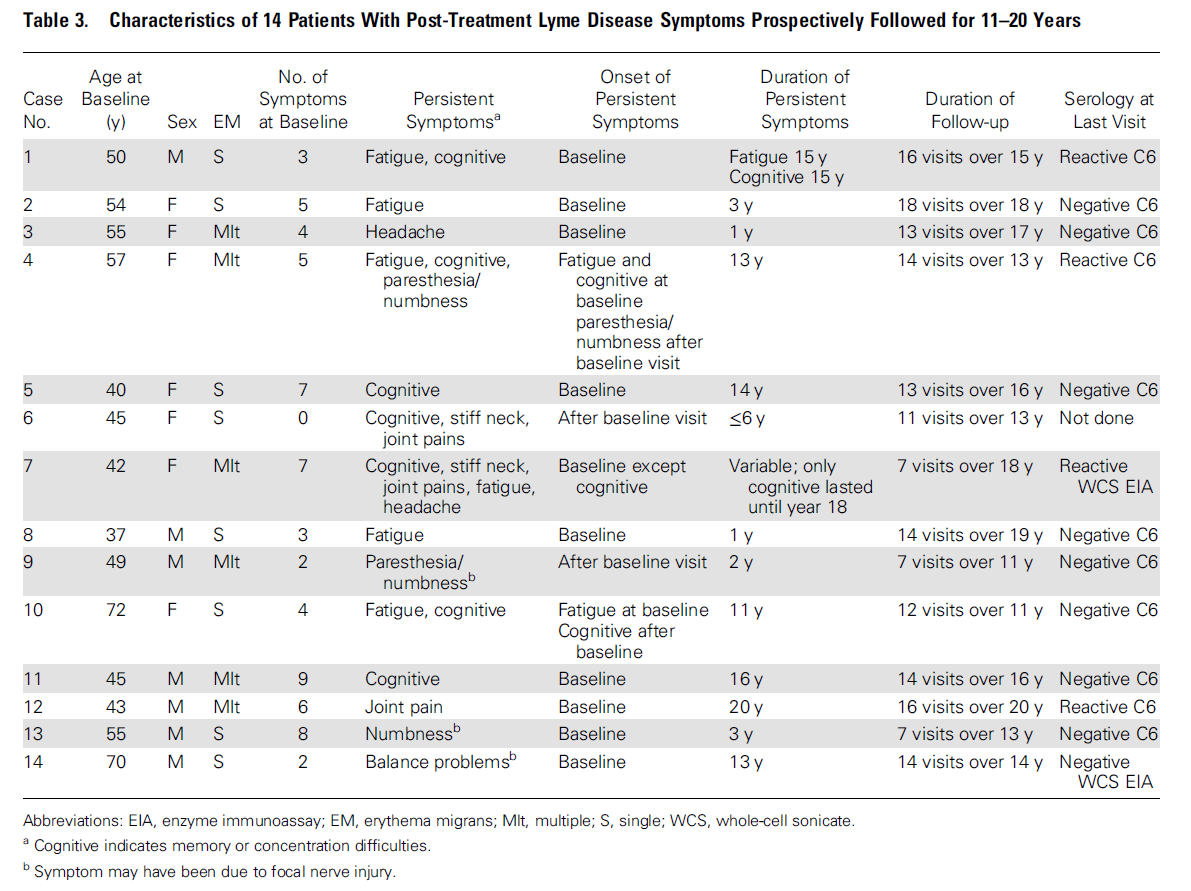
From the "Duration of Persistent Symptoms" column, we can calculate duration probabilities. All cases lasted at least a year, so p1y = 14/128 = 0.109. Assuming symptoms for case no. 6 lasted at least 5 years, p5y = 9/128 = 0.070. p10y = 8/128 = 0.063. And p20y = 1/128 = 0.008.
Apart from the qualifiers that this study itself gives, I have two caveats about these numbers, both of which suggest that my p1y, p5y, p10y, and p20y parameters might be somewhat too low:
- The overall fraction of patients with possible PTLDS (10.9%) is on the low end relative to the numbers in my above discussion of the p6m parameter. Patients in this study had pretty early treatment: "The mean ± SD number of days of illness until the baseline visit was 5.44 ± 6.69 days (median = 3 days; range = 0–42 days)" (pp. 2-3). So PTLDS outcomes were probably better than usual. Hence, it might make sense to inflate the p1y, p5y, p10y, and p20y numbers somewhat to account for the fact that, in practice, not everyone gets treated so early. I haven't inflated these parameters because I'm unsure how much to inflate them, but keep in mind that they may be too low.
- 6 of the 14 patients with possible PTLDS continued to have symptoms as of the last follow-up (p. 4), though not functionally impairing symptomsc. My impression is that the histories of these patients is cut off because the authors wanted to publish this study rather than continuing to wait and see what happened. Hence, I think the "Duration of Persistent Symptoms" values are too small for these 6 people.
S1m
I assume that Lyme disease is fairly debilitating during the first few weeks.
My dad gave me permission to quote his account of Lyme disease (personal communication, 15 Aug. 2016):
I had Lyme disease in late June 2009. I developed symptoms such as high fever, dizziness, disorientation and blurred vision. It was very scary, unlike anything I had ever felt with any other kind of fever or flu. I think I then went online to check for Lyme symptoms because I had a hunch, and they were consistent with what I had. Then I looked below my left shoulder and saw the red spot, an oval approximately 3 cm in diameter. This was on a Friday night. I went to the doctor the next morning and the doctor confirmed my case on the basis of my symptoms. He did a blood test, but told me that if this was my first case of Lyme disease, the results would not likely be positive because I had not had sufficient time to produce the antibodies. He started my on a month-long course of doxycycline. My symptoms were alleviated only slightly over the course of the next few days but within a week I was able to move around more freely. My eyesight was still blurry and I could only move around for a little while without need to sit, but after a couple weeks I was able to travel to Washington, DC, where we spent the 4th of July. I went back to work after we got back from vacation - a total of about three weeks out of work. That was the only time I experienced Lyme disease and I don't think I have experienced any lingering symptoms from that episode but it's hard to tell if some aches and pains I have (occasional sore left shoulder for example) might be a lingering symptom or just old age.
S1y and S>1y
This article explains:
There is a large spectrum of illness severity in PTLDS, from minor symptoms to a more severe illness that has been characterized by declines in health-related quality of life and mild to moderate cognitive deficits in some patients.23–25 In antibiotic treatment trials of ideally diagnosed and treated early Lyme disease, only 10% of patients were found to have low health-related quality of life,26 which may be related to fatigue.27 However, in patients identified after treatment in the community setting, the impact of PTLDS on health-related quality of life was much higher.24 The more severe end of this illness spectrum has been described in population-based studies, where patients often had delayed treatment, initial misdiagnosis, or nonideal initial therapy.9,11,16
This study has several big caveatsd and so should be taken with salt. It refers to PTLDS as chronic Lyme disease (CLD). The paper reports:
CLD patients reported the following ten symptoms as severe or very severe: fatigue (48.3%), sleep impairment (40.8%), joint pain (39.1%), muscle aches (36.1%), other pain (34.4%), depression (33.8%), cognitive impairment (32.3%), neuropathy (31.6%), headaches (22.7%) and heart-related issues (9.6%). [...]
In March 2013, 81.0% of the general population ages 25–54 were employed, compared with 45.9% of CLD respondents in that age range [...]. Approximately 42% of respondents reported that they stopped working as a result of Lyme disease (with 24% reporting that they received disability as a result of CLD), while 25% reported having to reduce their work hours or change the nature of their work due to Lyme disease. These figures compare with 6.3% of the USA population that is unable to work due to health problems and 3.1% that are limited in work due to health problems [...]. Those respondents who were able to continue working reported missing 15 days of work during the preceding 240-day work year, and they reported an inability to concentrate while at work (so-called presenteeism) during 42 days of work in the preceding year due to illness. [...]
Approximately 75% of survey respondents reported severe or very severe symptoms related to fatigue, joint pain, headaches, other pain, muscle aches, neuropathy, cognitive impairment, sleep impairment or mood impairment, and 63% reported more than one symptom as severe or very severe [...].
This study found 6 patients with persistent Lyme symptoms in their last follow-up visits, 11-20 years after initial treatment. The health outcomes were pretty good (p. 6):
None of the 6 subjects with persistent symptoms at their last visit had evidence of functional impairment caused by the symptoms and thus did not meet criteria for post–Lyme disease syndrome [1]. For 5 of these 6 subjects who provided their own assessment of their overall health status at their last visit, 3 stated that their health was very good or good. The single individual who stated that his health status was poor had multiple comorbidities that likely contributed to this assessment as the visual analogue scale score for the single residual symptom (ie, difficulty concentrating) was only 2.2 out of a maximum value of 8.
Consistent with these results, in prior analyses of several other measures of health status in our prospective study, the health-related quality of life of the 100 individuals who were assessed by the [36-item short-form General Health Survey version 2] SF-36v2 at their final study visit, including 5 of the 6 subjects with residual symptoms from PTLDS at that visit, was comparable with that of the general population [6].
The same study says (pp. 5-6):
For the 11 subjects with PTLDS who had a symptom severity score recorded at both the last visit and at the first visit that the symptom occurred, the mean ± SD score at the last visit was 2.89 ± 1.84 with a range of 0.3–6.6 based on a visual analogue scale (with possible scores of 0 to 8), compared with 3.35 ± 2.20 with a range of 0.6–7.1 (P = .54) at the first visit. [...]
Based on the first question on the SF-36v2 that 12 of the subjects with PTLDS completed, 9 (75%) characterized their health as good to excellent at that visit. Of the 3 subjects who characterized their health as fair to poor at their final visit, 1 did not have any symptom associated with their PTLDS at that visit, and for the other 2 the level of severity of the post-treatment Lyme disease symptoms was 2.2 and 6.1 (out of a maximum of 8), respectively. The first subject of the latter 2 also had a number of serious comorbidities, including post-traumatic stress disorder and a colovesical fistula.
Lyme disease may lower IQ. There are many anecdotal accounts of this, though I'm unsure what fraction of Lyme patients experience long-term IQ reductions. I worry whether, in addition to noticeable reductions in cognitive function accompanying severe cases of PTLDS, there are milder reductions in IQ that accompany other cases of Lyme? I also worry that if I were to get Lyme and then recover, I would have a nocebo effect in which I would wonder whether my IQ had been slightly impacted, which might itself affect my cognitive performance. Hopefully such a nocebo effect could eventually be overcome.
Time spent checking for ticks
T
This parameter may depend a lot on how careful you want to be. And how careful you want to be is probably affected by the general risk of ticks in your region. While the "time spent checking for ticks" part of my calculator isn't directly linked to the "risk of ticks" part, the numbers you enter into the "time spent checking" part are likely to have a positive correlation with the risk numbers.
Dr. Gary Wormser advises: "You should do a tick check every 24 hours if you've been outside. To do a good tick check, you really need a second person, because it's hard for you to see all the areas where the ticks could be biting you." Sometimes I do tick checks by myself using two handheld mirrors to see my back. Sometimes I ask someone else to check my back, but this may take more time because I have to coordinate with the other person.
You can reduce the productivity cost of checking for ticks if you do something else at the same time, such as listening to an iPod, which is what I do. On the other hand, listening to something means I concentrate slightly less well on checking for ticks, which means the process takes slightly longer in total.
Disclaimer
Insert standard disclaimer about this page not providing expert medical advice.
Let me know if you have comments or corrections on this calculator. To see the source code, view the source of this page and look for the calculate() function.
Todo
I haven't yet had the chance to read as much of the literature on this topic as I'd like, but I don't have time now to do so. Below is my todo list for this article to show some additional sources that I didn't check out fully yet.
1. Finish reading https://peerj.com/articles/322/ and make sure I didn't miss anything
2. Read:
http://link.springer.com/article/10.1007%2Fs11136-012-0126-6
http://ije.oxfordjournals.org/content/34/6/1340.full
http://www.ncbi.nlm.nih.gov/pubmed/8085687
3. Check the fine print on the following:
http://danielcameronmd.com/sick-for-years-with-post-treatment-lyme-disease-syndrome/
"Eleven percent of individuals followed for more than 11 years suffered from PTLDS. [4] Both women (12.3%) and men (9.9%) were sick with PTLDS. [4]"
"An NIH-sponsored trial reported Lyme encephalopathy patients were sick an average of 9 years. [1] Another study found a series of chronic neurologic Lyme disease patients were sick up to 14 years. [2]"
Footnotes
- The formula for L is (1-S1m) * p1m * 1/12 + (1-S1y) * [ p3m * (3-1)/12 + p6m * (6-3)/12 + p1y * (12-6)/12 ] + (1-S>1y) * [ p5y * (5-1) + p10y * (10-5) + p20y * (20-10) ]. (back)
- To see why this matters, consider the following. Suppose N people get tested for Lyme, and let p be the fraction of them who actually have Lyme. Of the p * N people with Lyme, up to 36% will falsely test as negative: 0.36 * p * N people. Of the (1-p) * N people without Lyme, 1% to 3% (say, 2%) will falsely test as positive: 0.02 * (1-p) * N people. As long as p is not very close to 0, the number of people falsely testing as negative will be greater than the number falsely testing as positive, which means "number of people testing positive" will be less than the actual number of people who have the disease. (back)
- "Of the 14 patients with PTLDS, none was considered to be functionally impaired because of PTLDS at their final study visit" (p. 5). (back)
-
- The authors appear to believe in chronic Lyme disease.
- The article makes an arithmetic error: "roughly 300,000 people (approximately 1% of the U.S. population)".
- The survey sampled participants "from individuals who participated in or visited Lyme disease patient-centered online forums in which the survey was posted or publicized", which means that, as the authors acknowledge, "our sample is self-selected from participants who are sick enough (and Internet-savvy enough) to seek online support for their illness." I would guess that this dramatically skews the results of the survey.
- The sample includes lots of people with very late diagnosis: "7.9% of respondents were not diagnosed until at least 3 months after the onset of symptoms, 16.6% were not diagnosed for at least 6 months, and 61.7% were not diagnosed for at least 2 years. Approximately half (50.5%) of the sample reported having Lyme disease for more than 10 years."